Severe Covid in young people can mostly be explained by obesity – new study
By Nerys M Astbury, University of Oxford; Carmen Piernas, University of Oxford, and Min GAO, University of Oxford
From the start of the pandemic, it was clear that some people who were infected with the coronavirus were experiencing more severe illness, which increased their chances of being hospitalised, admitted to an intensive care unit (ICU) or dying.
As we age, a weaker immune system and chronic health conditions could influence the way our body responds to the virus. Indeed, age is the biggest risk factor for developing severe COVID or dying from it. Over 70% of deaths attributed to COVID in the UK are in those aged 75 years and over.
Ethnicity, sex and obesity were also found to be risk factors for severe COVID outcomes. But, of course, we can’t do anything about our age, sex or ethnicity. We can do something about being overweight, though.
Body mass index (BMI) is a measure applying height and weight to calculate a weight score. A person with a BMI over 25 is considered to be overweight, and over 30 is considered to be obese.
Pikovit/Shutterstock
Early studies reported that many more people who were overweight or obese were admitted to an ICU and needed mechanical ventilation than people who were not overweight or obese. Indeed, even Prime Minister Boris Johnson attributed the severity of his own COVID infection to the fact he was “way overweight” at the time.
A study published last year in Nature reported that obesity increased the risk of COVID-related death substantially. People with the highest BMI (over 40) were at 92% higher risk of dying from COVID compared with people with a healthy BMI (18.5-25). But most people are not this overweight. Many people have been inactive during the lockdowns and may have gained a bit of extra weight, so could that excess weight also increase the risk of developing severe COVID? Our latest study looked at just that.
Using the anonymous health records from almost 7 million people aged 20-99 years in England, we explored the risk of severe COVID across the full BMI range.
Of the 6,910,695 people who had their weight recorded, 13,503 were admitted to hospital with COVID, 1,602 needed treatment in an ICU, and 5,479 died of COVID during the first wave in the UK (January-May 2020). Most of these people were aged over 60 (72% of hospital admissions, 56% of ICU admissions and 93% of deaths).
Risk starts to increase at high-end of healthy weight
We found that the lowest risk was found among those with a BMI of 23, at which point the risk increased linearly, around 5% higher risk of hospital admission, 10% higher risk of ICU admission, and 4% of death per each unit increase in BMI.
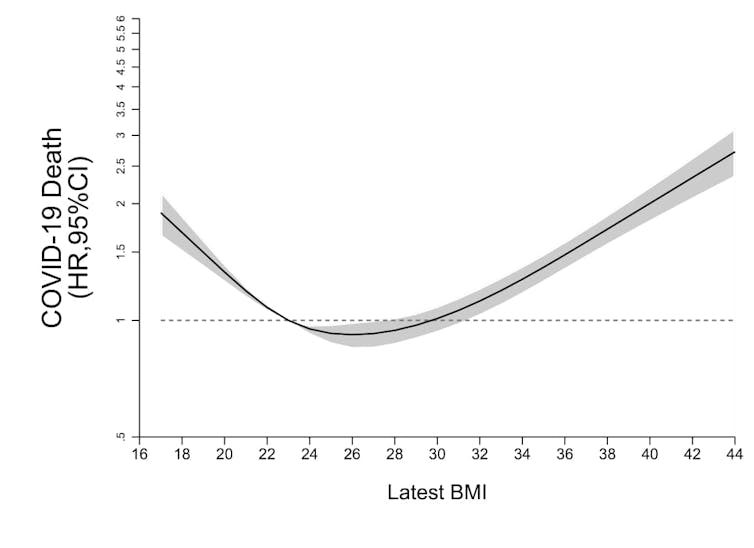
The Lancet Diabetes & Endocrinology
Our analysis took into account several factors that might influence risk, such as age, sex, ethnicity and existing health conditions, including type 2 diabetes. People with a BMI under 23, which includes people who are underweight (BMI below 18.5) were also at risk of COVID-related hospital admission and death. This could be linked to frailty associated with having a low body weight.
Notably, the effect of excess weight on the risk of severe COVID was greatest in young people aged 20 to 39 years of age, and decreased after age 60. Excess weight had very little effect on the risk of severe COVID in people aged over 80 years.
The increase in the risk of hospitalisation per BMI unit for those aged 20-39 is 9%; for those aged 40-59, 8%; for 60-79 years, 4%; and 1% for people aged 80-99 years. The increase in the risk of death per BMI unit for those aged 20-39 is 17%; for those aged 40-59, 13%; for 60-79 years, 3%; and 0% for people aged 80-99 years.
Younger people generally experienced much less severe COVID and were less likely to die compared with older people. Still, a younger person with a BMI of 30 would have a much higher risk of severe COVID than their healthy weight peers.
The risks associated with higher BMI were greater for black people compared with white people. The increase in the risk of hospitalisation per BMI unit for black people was 7% compared with 4% for white people. And the increase in the risk of death for black people was 8% versus 4% for white people. There was no evidence that the risks for other ethnic groups differed from those of the white populations.
Many good reasons to lose weight
Although we couldn’t look to see if losing weight could reduce these risks in this study, it is plausible that shedding excess weight could help reduce the risk of developing severe COVID. And, of course, losing weight has other health benefits too.
But losing weight is hard. We need more support systems to help people lose weight. This could help reduce the severity of COVID at a population level, which may help reduce the burden on healthcare systems, while also reducing the risks for heart disease, type 2 diabetes and some cancers.![]()
Nerys M Astbury, Senior Researcher, Diet and Obesity, University of Oxford; Carmen Piernas, University Research Lecturer, Nutrition, University of Oxford, and Min GAO, PhD Candidate, Non-communicable Chronic Disease, University of Oxford
This article is republished from The Conversation under a Creative Commons license. Read the original article.